Gestational Diabetes self-care: Dietitian approved opinions.
Gestational diabetes mellitus (GDM) can happen during pregnancy. Not every pregnancy faces GDM, but a large number of would-be mothers face this challenge during pregnancy.
Table of Contents
ToggleA diagnosis of gestational diabetes during pregnancy can feel overwhelming. It can bring a wave of questions and concerns. But it’s also an opportunity. A chance to take an active, empowered role in your health and the well-being of your baby.
This condition is a temporary type of diabetes. It occurs during pregnancy. The Centers for Disease Control and Prevention reports that the percentage of mothers diagnosed with gestational diabetes is continuously rising. It rose from 6.0% in 2016 to 8.3% in 2021. You are not alone in this journey, and with the right knowledge and tools, you can manage it effectively.
If you’ve been diagnosed with gestational diabetes, you have some good news. With proper self-care and medical guidance, you can have a healthy pregnancy and a healthy baby.
Understanding The Diagnosis: What Gestational Diabetes Means for You
A gestational diabetes diagnosis means your body is not producing enough insulin. Insulin is needed to manage the glucose (sugar) in your blood.
It is a common effect of pregnancy hormones. Your body and your baby need glucose for energy and growth. But excessively high blood sugar levels can lead to complications.
It usually appears in the second or third trimester and typically resolves after childbirth. However, it requires careful management because uncontrolled blood sugar can increase the risk of:
- High birth weight of the baby
- Complications during delivery (e.g., C-section)
- Low blood sugar in newborns
- Increased risk of type 2 diabetes for both mother and child later in life
The primary goal of management is to keep your blood sugar within a healthy range. It is for ensuring a safe and healthy pregnancy for both of you.
Why Self-Care is Your Most Powerful Tool During Pregnancy
Gestational diabetes self-care is the cornerstone of managing this problem. It’s not about perfection. It’s about making consistent, conscious choices that support your health.
Gestational diabetes self-care means doing management through diet, physical activity, and monitoring. This way, you can directly influence your blood glucose levels.
This proactive approach mitigates potential risks. It also builds a foundation for lifelong healthy habits. It is the first step to reduce your future risk of developing type 2 diabetes.
Why Self-Care is Your Most Powerful Tool During Pregnancy
Gestational diabetes self-care is the cornerstone of managing this problem. It’s not about perfection. It’s about making consistent, conscious choices that support your health.
Gestational diabetes self-care means doing management through diet, physical activity, and monitoring. This way you can directly influence your blood glucose levels.
This proactive approach mitigates potential risks. It also builds a foundation for lifelong healthy habits. It is the first step to reduce your future risk of developing type 2 diabetes.
Gestational Diabetes Self-care: The Basics You Need to Know
Knowledge is the first step toward empowerment. Understanding what gestational diabetes is, why it occurs, and how it’s identified will demystify the condition. It will give you the confidence to manage it effectively.
What is Gestational Diabetes (GDM)?
Gestational Diabetes Mellitus (GDM) is a condition characterized by high blood sugar. It develops during pregnancy and usually disappears after giving birth. During pregnancy, the placenta produces hormones that help the baby grow. These same hormones can block the action of the mother’s insulin, a phenomenon called insulin resistance.
While most pregnant women can produce more insulin to overcome this resistance, some can’t. When the body can’t make or use enough insulin things get complicated. Insulin works to move glucose from the blood into the cells for energy. blood sugar levels rise. This situation is called GDM.
Common Gestational Diabetes Risk Factors
While any woman can develop GDM, certain factors increase the risk. These include:
- Being overweight or obese before pregnancy
- A personal or family history of diabetes
- Having had GDM in a previous pregnancy
- Being over the age of 25
- Belonging to certain ethnic groups (e.g., African American, Hispanic, Asian American)
- Having polycystic ovary syndrome (PCOS)
- Previously giving birth to a baby weighing more than 9 pounds
It’s important to note that many women with GDM have no obvious risk factors. This is why screening is a routine part of prenatal care.
How Gestational Diabetes is Diagnosed
GDM is typically diagnosed between the 24th and 28th weeks of pregnancy through a glucose tolerance test. The process usually involves two steps:
Glucose Challenge Test:
You’ll drink a sugary liquid, and your blood will be drawn one hour later to measure your blood glucose level. If the level is high, it indicates a potential issue with glucose processing.
Oral Glucose Tolerance Test (OGTT):
If the initial test is abnormal, you’ll undergo a longer test. This requires fasting overnight. Then, having your blood drawn before and at several intervals after drinking a more concentrated glucose solution. This test provides a definitive diagnosis by showing how your body handles a large glucose load over time. A study using this one-step approach found that the prevalence of GDM rose from 14.0% to 25.3% between 2012 and 2022, highlighting its increasing detection.
Self-Care Strategies for Gestational Diabetes
Most GDM women become cured after delivery. But after delivery around 20% to 50% have a chance of developing type 2 diabetes. It will happen in the next 5 to 10 years.
To reduce the risk of developing subsequent diabetes, it is recommended to modify the lifestyle. /One is reducing the weight or preventing more weight gain. Another is increasing physical exercise. Both of these are important to prevent the development of type 2 diabetes.
1. Monitoring Your Blood Sugar Regularly
Once diagnosed, monitoring your blood sugar is the most crucial daily task. It provides real-time feedback on how your body responds to food, activity, and stress. Allows you and your healthcare team to make adjustments to your management plan.
The Importance of Self-Monitoring Blood Glucose (SMBG)
Self-monitoring blood glucose (SMBG) is a good system for self-care. It will give you the exact picture of your blood glucose level. Regular testing reveals blood glucose patterns. It helps you understand the immediate impact of your choices.
Did that meal cause a spike?
Did that walk help lower your numbers?
This information is vital for adjusting your diet and exercise routines to maintain stable blood sugar levels. Also, protecting both your health and your baby’s development.
Your Blood Glucose Monitoring Toolkit
Your healthcare provider will prescribe a blood glucose meter. It is also known as a glucometer. Your essential toolkit will include:
- Glucometer: The device that reads your blood sugar.
- Test Strips: Small strips that absorb a blood sample and are inserted into the meter.
- Lancet Device and Lancets: A spring-loaded device that holds a small needle (lancet). It is for pricking your finger for a blood sample.
- Logbook or App: A place to record your readings, meals, and activities.
Your provider or a diabetes educator will teach you how to use the equipment correctly and how often to test. This is typically the first thing in the morning (fasting) and one or two hours after each meal.
Interpreting Your Blood Glucose Readings
Your healthcare team will provide you with target blood sugar ranges. While these can vary slightly, common targets are:
- Fasting (before breakfast): 95 mg/dL or less
- One hour after meal: 140 mg/dL or lower
- Two hours after meal: 120 mg/dL or lower
Regular high readings indicate that your current plan needs adjustment. It can involve changes to your diet, exercise, or, in some cases, medication like insulin.
Conversely, readings that are too low (hypoglycemia) also need attention.
Maintain a logbook or use a digital app to track progress.
Consistency is key. Regular monitoring helps detect fluctuations and adjust your diet or activity accordingly.
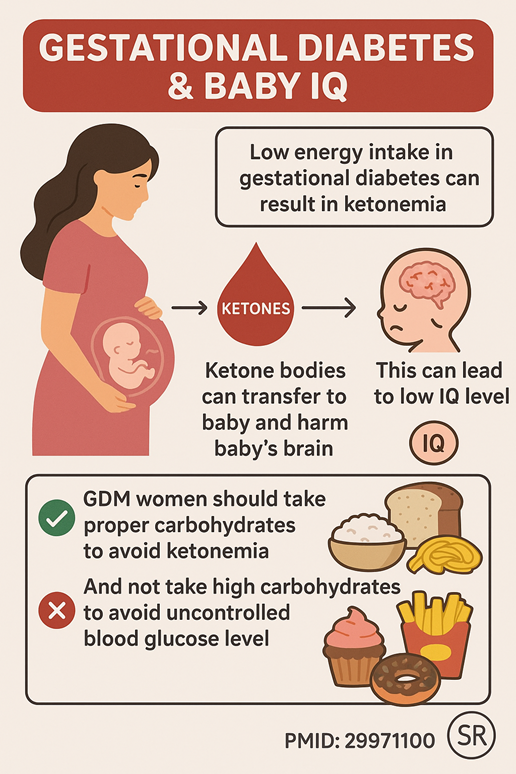
Monitoring for Ketones: When and Why it’s Important
Ketones are substances made when the body breaks down fat for energy instead of glucose. During pregnancy, it’s important to avoid high levels of ketones.
If you take less amount of food to avoid a higher blood sugar level, GDM patients develop ketosis. This situation is potentially harmful to the baby. Studies show GDM mothers’ ketonemia results in lower IQ in the baby in later life.
Your doctor may ask you to test your urine for ketones. Especially if your fasting blood sugar is high or if you are not gaining enough weight. This ensures your body and baby are getting enough energy from carbohydrates and that your diet is properly balanced.
2. Follow a Balanced Diet Plan
Nutrition plays a vital role in managing gestational diabetes. A dietitian or healthcare provider can customize a plan, but general guidelines include:
Each meal and snack should be a combination of all nutrients.
Complex carbohydrates, lean protein, and healthy fats should all be there. They work together to slow down digestion and the absorption of glucose.
It prevents sharp spikes in blood sugar. Eating smaller, more frequent meals also helps maintain stable energy and glucose levels throughout the day. Three main meals and two to three snacks is very helpful. The meals should be with adequate carbohydrate, protein, fat, and vitamins, and minerals will help to control blood sugar effectively.
Navigating Carbohydrates: The Key to Blood Sugar Management
Carbohydrate foods directly impact the level of blood sugar. The key is to choose complex, high-fiber carbohydrates over simple, processed ones.
- Complex Carbs (Choose these): Whole grains (oats, quinoa, brown rice), beans, lentils, and starchy vegetables (sweet potatoes, corn). Their fiber slows down the conversion to glucose.
- Simple Carbs (Limit these): Sugary drinks, white bread, pastries, and candy. These are absorbed quickly, causing rapid blood sugar spikes. Portion control is equally critical. Your dietitian will help you determine the right amount of carbohydrates for each meal and snack.
A proper amount of carbohydrate against insulin intake will help you to a stable sugar level. It will also prevent hypoglycemia (critically lowered blood sugar).
Foods to Prioritize for Optimal Health
Focus on nutrient-dense foods that support a healthy pregnancy and stable blood sugar:
- Portion Control: Eat smaller, more frequent meals instead of 2–3 large meals.
- Lean Proteins: Chicken, fish, tofu, eggs, and legumes.
- Healthy Fats: Avocado, nuts, seeds, and olive oil.
- Non-Starchy Vegetables: Vegetables, Leafy greens, broccoli, peppers, and cucumbers.
- Fiber-Rich Fruits: Berries, apples, and pears (in moderation).
Foods to Limit or Avoid
To manage blood sugar, it’s best to significantly limit or avoid:
- Sugary Beverages: Soda, sweetened teas, and fruit juice.
- Processed Foods: Packaged snacks, fast food, and foods with added sugars.
- Refined Grains: White rice, white pasta, and white bread.
- Sweets and Desserts: Cakes, cookies, and ice cream.
Practical Meal Planning and Preparation Strategies
Success with a gestational diabetes self-care often comes down to good diet planning.
- Plan Meals Weekly: Decide what you’ll eat for the week to avoid last-minute, unhealthy choices.
- Prepare the Ingredients: Wash and chop vegetables, cook grains, and portion out proteins. Once you prepare them in advance, it will be easier for you to take these foods.
- Read Labels: Pay attention to serving sizes and total carbohydrate counts on packaged foods.
- Balance Your Plate: Aim for a plate that is half non-starchy vegetables, one-quarter lean protein, and one-quarter complex carbohydrates.
Partnering with a Dietitian or Nutritionist
Working with a registered dietitian is invaluable. They can create a personalized meal plan tailored to your food choices, cultural background, and specific glucose targets. A personalized meal plan also ensures the extra energy servings to nurture the baby well in your womb.
They will help you to understand low glycemic index foods to choose. You can become satisfied, as well as you can control your blood sugar levels. They will make you easily understand.
They provide education, support, and practical strategies to help you navigate your nutritional needs with confidence.
3. Stay Physically Active: Safe and Effective Movement
Alongside diet, regular physical activity is a powerful tool for managing GDM. Exercise helps your body use insulin more effectively, which in turn helps lower your blood sugar levels.
The Benefits of Exercise for Gestational Diabetes Management
Regular physical activity during a GDM pregnancy offers numerous benefits. It improves insulin sensitivity. It means your cells are much better able to use glucose for energy.
This directly contributes to lower blood glucose readings. Exercise also helps manage weight gain, reduces stress, and can improve sleep quality—all of which support a healthier pregnancy.
Safe Exercise During Pregnancy with GDM
Most women with GDM can and should exercise. Safe and effective options include:
- Walking: A simple, low-impact activity that is easy to start. Aim for a brisk 10-15 minute walk after each meal.
- Swimming or Water Aerobics: The water supports your weight, reducing strain on joints.
- Stationary Cycling: A safe way to get a cardiovascular workout.
- Prenatal Yoga or Pilates: These can improve flexibility, strength, and stress levels.
Integrating Physical Activity into Your Daily Life
Consistency is more important than intensity. Find activities you enjoy and schedule them into your day. Even small bursts of movement count. Park further away, take the stairs, or do gentle stretches during TV commercials. The goal is to aim for about 30 minutes of moderate activity on most days of the week.
When to Consult Your OBGYN About Exercise
Always discuss your exercise plan with your healthcare provider before starting. They can confirm which activities are safe for you. You should stop exercising and contact your doctor if you experience specific symptoms. They may experience vaginal bleeding, dizziness, chest pain, contractions, or very high blood sugar readings.
4. Maintaining Healthy Weight Gain
Weight gain during pregnancy is normal, but with gestational diabetes, it’s important to avoid excessive gain. Follow your doctor’s recommendations for healthy weight targets based on your BMI before pregnancy.
There are indications for weight gain. If you are underweight, weight gain should be 12 to 18 kg. If you are of normal weight gain should be 11 to 16 kg. If you are overweight, weight gain should be maximum 11 kg.
It depends on your pre-pregnancy weight. Hence, you should consult with your physician and dietitian as well.
Your dietitian will help you to make personalized meal plans to achieve targeted weight gain.
5. Manage Stress Levels: Holistic Self-Care Strategies
Managing gestational diabetes effectively also involves caring for your mental and emotional well-being. Stress and lack of sleep can negatively impact blood sugar levels. Reducing stress and getting proper sleep can help you manage your blood sugar levels effectively.
Managing Stress and Emotional Well-being
A GDM diagnosis can be stressful. Chronic stress raises cortisol levels, which can, in turn, elevate blood sugar. Incorporate stress-reduction techniques into your daily routine, such as deep breathing exercises, mindfulness, meditation, or spending time in nature.
Technology can also play a supportive role. One study in Brieflands found that WhatsApp-based self-care education significantly improved post-meal blood glucose levels. If your healthcare provider gives you access to an online support group invitation, you can join. And can get benefits from those groups.
Prioritizing Quality Sleep
Sleep deprivation can worsen insulin resistance. Aim for 7-9 hours of quality sleep per night. Establish a relaxing bedtime routine, avoid screens before bed, and create a comfortable sleep environment. If pregnancy discomfort makes sleep difficult, talk to your provider about safe solutions.
The Importance of Self-Compassion and Support Systems
Be kind to yourself. You will have days when your blood sugar numbers are not perfect. This is normal. Focus on progress, not perfection. Lean on your support system—your partner, family, and friends. You can connect with other women who have GDM. Either online or in a local support group can also provide invaluable encouragement and understanding.
Partnering with Your Healthcare Team: Your Network of Support
You are the leader of your self-care, but you are not alone. Your healthcare team is your dedicated network of support, providing the expertise and guidance needed to navigate your pregnancy safely. This team may include your OBGYN, a maternal-fetal medicine specialist, a registered dietitian, and a certified diabetes educator.
Open communication, regular appointments, and adherence to their medical advice are essential. They will monitor your blood glucose and also other important factors. Such as blood pressure, as GDM can increase the risk of high blood pressure during pregnancy.
6. Take Medications or Insulin if Prescribed
Sometimes, lifestyle changes alone may not be enough.
Without obvious explanations from food records, if glucose level remains elevated for 1-2 weeks consistently, insulin is needed.
Not all GDM women need drugs or insulin.If 2 consecutive weeks are passed with proper dietary approaches and physical activities but there are no improvements of high blood glucose. Then insulin or metformin or glyburide is given to control the hyperglycemia. It is to be given by your doctor.
If your doctor prescribes insulin or oral medications, take them exactly as directed. Never skip doses without medical advice.
If you are on insulin, there could be a potential problem with hypoglycemia or low blood sugar.
To avoid a low blood sugar level, take 3 major meals with 2 small snacks a day. Never skip meals, as this can cause hypoglycemia severely.
7. Stay Hydrated
Drinking enough water supports kidney function and helps the body maintain stable blood sugar levels. Aim for 8–10 glasses of water per day unless your doctor recommends otherwise.
During pregnancy, proper hydration can help you poop easily. It can also reduce the chance of having urinary tract infection or UTI. If you have UTI, it is difficult to prescribe antibiotics as you are carrying a baby inside you. It is better to prevent UTI at this time. So, stay hydrated adequately.
8. Regular Check-Ups
Frequent prenatal visits allow your healthcare provider to monitor your blood sugar, baby’s growth, and overall pregnancy health. Ultrasounds and other tests may be suggested to ensure everything is on track.
Life After Delivery
For most women, gestational diabetes goes away after childbirth. However, self-care should continue even postpartum:
- Get your blood sugar tested 6–12 weeks after delivery.
- Continue healthy eating and physical activity.
- Maintain a healthy weight to reduce the risk of developing type 2 diabetes in the future.
- Breastfeeding can help regulate your metabolism and benefit your baby’s health.
Final Thought
A diagnosis of gestational diabetes is a call to action. An invitation to become deeply involved in your health and your baby’s. By embracing empowered self-care, you can effectively manage your blood sugar levels. It can be achieved through mindful nutrition, consistent physical activity, and diligent monitoring. Remember to manage stress, prioritize sleep, and lean on your healthcare team and personal support systems.
This journey provides an opportunity to build healthy habits that can last a lifetime. After birth, it is crucial to follow up with your doctor for postpartum screening. Women with a history of GDM have an approximately tenfold higher risk of developing type 2 diabetes later in life. The skills you learn and the healthy lifestyle you adopt now are powerful tools for protecting your long-term health.
You have the strength and capability to manage this condition, ensuring a healthy outcome for both you and your baby.
FAQ:
1. What is gestational diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy. Pregnancy itself changes several hormonal responses; some women may develop gestational diabetes. It leads to high blood sugar levels, which may result in complications for both mother and baby.
2. Who is at risk of developing gestational diabetes?
You may be at higher risk if you:
- Are overweight or obese
- Have a family history of diabetes
- Had gestational diabetes in a previous pregnancy
- Are older than 25 years
- Have polycystic ovary syndrome (PCOS)
- Gave birth to a baby weighing more than 4 kg (9 lbs.) before
3. What causes gestational diabetes?
During pregnancy, hormones like estrogen and cortisol can make your body’s cells less responsive to insulin. This situation is called insulin resistance. If your pancreas cannot produce enough insulin to overcome this resistance, blood sugar levels rise. It leads to gestational diabetes and further complications.
4. How is gestational diabetes diagnosed?
It’s usually diagnosed between 24–28 weeks of pregnancy through an oral glucose tolerance test (OGTT). Some women at higher risk may be tested earlier.
5. How can gestational diabetes be managed?
Most women can manage it through:
- A healthy, balanced diet with appropriate calorie intake.
- Regular physical activity as recommended by a doctor.
- Monitoring blood glucose levels regularly.
- Medication or insulin therapy if lifestyle changes aren’t enough to control blood sugar levels.
6. What are safe exercises during gestational diabetes?
Moderate activities like walking, swimming, prenatal yoga, or stationary cycling are usually safe. Minimum 30 minutes exercises help to reduce insulin resistance during this time. Always consult your healthcare provider before starting or continuing exercise.
7. Can gestational diabetes affect my baby?
If gestational diabetes is uncontrolled, it can cause:
- Large birth weight (macrosomia)
- Preterm birth
- Breathing difficulties in the newborn
- Low blood sugar of the baby after birth and death from it.
However, with proper management, most women have healthy pregnancies and babies.
8. What foods should I eat if I have gestational diabetes?
Choose:
- Whole grains, vegetables, fruits with low glycemic index
- Lean proteins (chicken, fish, lentils, eggs)
- Healthy fats (avocado, olive oil, nuts)
- Avoid refined carbs, sugary drinks, and processed foods.
Always control the food portions to avoid sugar spike. You should consult with your dietitian to know how much is safe portions for you.
9. Will gestational diabetes go away after delivery?
Usually blood sugar levels return to normal after childbirth. But women with GDM are at higher risk of developing type 2 diabetes later in life. A healthy lifestyle may reduce the chance of having type 2 diabetes later in life.
A follow-up glucose test is usually done 6–12 weeks postpartum.
10. How can I prevent gestational diabetes in future pregnancies?
- Maintain a healthy weight before pregnancy
- Eat a balanced diet rich in fiber and low in added sugars
- Stay physically active
- Get regular health checkups

B.Sc, M.Sc (Food And Nutrition) (DU)
Clinical Dietitian and Nutritionist.
Lubana General Hospital & Cardiac Center.
Dhaka, Bangladesh.

